Abstract
Intrahepatic cholestasis of pregnancy (ICP) affects 1/140 UK pregnancies; with pruritus, hepatic impairment and elevated serum bile acids. Severe disease is complicated by spontaneous preterm delivery and stillbirth. Previous studies have reported mutations in hepatocellular transporters (ABCB4, ABCB11). High throughput sequencing in 147 patients was performed in the transporters ABCB4, ABCB11, ATP8B1, ABCC2 and tight junction protein 2 (TJP2). Twenty-six potentially damaging variants were identified with the following predicted protein changes: Twelve ABCB4 mutations - Arg47Gln, Met113Val, Glu161Gly, Thr175Ala, Glu528Glyfs*6, Arg590Gln, Ala601Ser, Glu884Ter, Gly722Ala, Tyr775Met (x2), Trp854Ter. Four potential ABCB11 mutations - Glu297Gly (x3) and a donor splice site mutation (intron 19). Five potential ATP8B1 mutations - Asn45Thr (x3), and two others, Glu114Gln and Lys203Glu. Two ABCC2 mutations - Glu1352Ala and a duplication (exons 24 and 25). Three potential mutations were identified in TJP2; Thr62Met (x2) and Thr626Ser. No patient harboured more than one mutation. All were heterozygous. An additional 545 cases were screened for the potential recurrent mutations of ATP8B1 (Asn45Thr) and TJP2 (Thr62Met) identifying three further occurrences of Asn45Thr. This study has expanded known mutations in ABCB4 and ABCB11 and identified roles in ICP for mutations in ATP8B1 and ABCC2. Possible novel mutations in TJP2 were also discovered.
Similar content being viewed by others
Introduction
Intrahepatic cholestasis of pregnancy (ICP), also called obstetric cholestasis, is the commonest pregnancy-specific liver disease. Typically presenting in the third trimester, ICP can be debilitating for the mother and threaten the health of the fetus1,2,3. Affected women have abnormal values of hepatobiliary-injury biomarkers, including raised serum bile acid (BA) concentrations4, that typically resolve by 12 weeks postpartum. Adverse pregnancy outcomes occur more commonly when maternal serum bile acid concentrations are >40 µmol/L. They include spontaneous preterm labour, prolonged admission to the neonatal intensive care unit and third trimester intrauterine death2,3,5,6. ICP is associated with a disrupted metabolic profile7,8 and can have long-term consequences for the health of the mother9,10 and child11.
The aetiology of ICP is complex and not fully understood, but a role has been established for the effect of elevated reproductive hormones towards the end of pregnancy (estrogens and sulphated progesterone metabolites), when the disease most commonly presents (12,13, reviewed in ref.14). Indications of genetic involvement in disease susceptibility are clear (reviewed in ref.15). Pedigree studies have identified families where ICP is inherited in an autosomal dominant sex-limited fashion16,17. The varying geographical prevalence also indicates genetic involvement, with population-specific genetic backgrounds conferring different levels of risk18. Historically the prevalence of ICP was highest amongst the Native Chilean population19. Further evidence of genetic involvement comes from sibling studies that show a 12-fold increase in risk between parous sisters20,21.
Severe childhood liver disease can be caused by homozygous mutations in genes that encode transporters involved in bile formation at the hepatocyte canalicular membrane. These transporters play roles in cholestatic disorders that range in severity from progressive paediatric disease to transient cholestasis associated with drug ingestion or pregnancy (ICP)22.
Studies of the gene ABCB4, (ATP binding cassette subfamily B member 4) encoding the phosphotidylcholine floppase MDR3 and homozygously mutated in progressive familial intrahepatic cholestasis (PFIC) type 3, identified a heterozygous mutation of ABCB4 first in a familial case23 and then in a sporadic instance of ICP24. Subsequent studies have identified a wide range of mutations of ABCB4 in ICP, most commonly missense mutations15. Approximately 10% of women with ICP harbour a mutated allele of ABCB4 15. Mutations of ABCB4 have also been implicated in drug-induced cholestasis25 and low phospholipid-associated cholelithiasis26.
The bile salt export pump (BSEP), encoded by the gene ABCB11, (ATP binding cassette subfamily B member 11) is homozygously mutated in PFIC type 2 and benign recurrent intrahepatic cholestasis (BRIC) type 227. Several studies found ABCB11 mutations in women affected with ICP28,29,30.
Of note is that in addition to causative mutations of ABCB4 and ABCB11 acting as Mendelian-like alleles, population studies of ICP cohorts have identified common genetic variants at these loci that contribute to disease risk, albeit to a much smaller degree than causative mutations31.
The third PFIC (and BRIC) gene, ATP8B1, (ATPase class 8B member 1) encoding a phosphatidyl serine flippase (familial intrahepatic cholestasis 1, FIC1), has only been studied to a limited extent (with respect to sequencing) in ICP cohorts, and hence the role of genetic variation at this locus in ICP is not established32,33. A functional interdependence of this flippase with MDR3 in hepatocytes suggests that ATP8B1 remains a viable candidate for involvement in ICP susceptibility34, as does the link to ABCB11 function through FXR/PLD2 signalling35.
Another canalicular ATP-driven transporter, the multidrug resistance-associated protein 2 (MRP2, encoded by the gene ABCC2(ATP binding cassette subfamily C member 2) is involved in bile formation. This protein exports bilirubin, some bile acids and many other anion conjugates into bile. Homozygous mutations of ABCC2 cause the rare liver disorder Dubin-Johnson syndrome, which presents with conjugated hyperbilirubinaemia36. Although common variation and ICP susceptibility have been investigated at this locus in population cohorts, with conflicting results31,37,38, there are no published analyses of comprehensive sequencing of the coding region of ABCC2 in an ICP cohort.
Familial forms of severe progressive cholestasis without a confirmed genetic diagnosis also exist39. Mutations of another gene, tight junction protein 2 (TJP2) have recently been implicated in some patients with such disease40. The encoded protein named zona occludens 2 (ZO-2) is a cytosolic component of a number of types of cell-cell junctions at many sites, interacting with membrane proteins and cytoskeletal proteins. The detergent actions of bile acids in the liver on mutated cellular junctions are postulated to cause the cholestatic phenotype40. To date this gene has not been studied in ICP. Given the role of other PFIC genes in ICP, TJP2 seems a reasonable candidate for analysis.
To clarify the extent of involvement in ICP of these genes implicated in familial cholestasis we undertook high-throughput targeted sequencing of ABCB4, ABCB11, ATP8B1, ABCC2 and TJP2 in a cohort of 147 women with ICP.
Patients
The study included 147 women with a confirmed diagnosis of ICP, recruited through the Women’s Health Research Centre at Queen Charlotte’s and Chelsea Hospital, Imperial College Healthcare NHS trust, St. Mary’s Hospital Imperial College London, and North Lincolnshire and Goole Hospitals NHS foundation trust. All patients provided written informed consent, conforming to the 1975 Helsinki guidelines; permission for the study was granted by the ethics committee of the Hammersmith Hospitals NHS Trust, London (references REC97/5197 and 08/H0707/21).
ICP was diagnosed as described previously on the basis of clinical symptoms (pruritus without identifiable skin lesions other than excoriations) and routine laboratory investigations33. ICP was confirmed with detection of raised maternal serum bile acids. Women were excluded if viral or autoimmune hepatobiliary disease was diagnosed. A larger cohort of 545 patients with ICP, described in a previous study31, was used to evaluate potential recurrent mutations.
Results
Genes implicated in familial cholestasis underwent targeted next-generation sequencing using the MiSeq platform in a cohort of 147 ICP patients. This identified 26 potentially pathogenic variations. Table 1 shows each variant identified together with its predicted protein consequence. Clinical findings for each patient in whom a potential mutation was identified are also shown (Table 2). All of the described mutations were observed in the heterozygous state and no patient harboured more than one potentially pathogenic variant. The frequency of two of the previously identified common susceptibility variants for ICP31; namely rs2109505 in ABCB4 and rs2287622 in ABCB11, was noted in these individuals (Table 1). All of the missense variants identified, except where specified (Table 1) were predicted to be pathogenic by SIFT and MutationTaster.
ABCB4 variants
Consistent with previous findings15, the largest number of potential mutations (11 different variants in 12 patients) were identified in the gene encoding the phosphatidyl choline floppase ABCB4 in this patient cohort (Table 1). Two predicted resulting variants, namely Thr175Ala and Arg590Gln, have previously been reported as pathogenic in cholestatic disease41,42. Three novel mutations are predicted to result in a frameshift leading to a stop codon six missense amino acids thereafter (Glu528Glyfs*6) and two immediate introductions of a premature stop codon (Glu684Ter, Trp854Ter), a type of mutation only very infrequently previously described in ICP15. The remaining 7 mutations are novel missense changes predicted to be pathogenic (Alamut).
ABCB11 variants
Fewer potentially pathogenic variants (n = 2, 4 patients) were identified in ABCB11, encoding the bile salt export pump. A recurrent mutation, predicted to yield the substitution Glu297Gly, first described in PFIC2 patients27, and later identified in a study of ICP patients29, was discovered in 3 separate patients not known to be related. A donor splice site mutation in intron 19 was identified with the predicted consequence of an exon skipping event. A missense variation, resulting in the protein change Asn591Ser (dbSNP: rs11568367), was identified in an additional patient, which has previously been reported in ICP28. However, despite this amino acid being highly conserved, bioinformatic tools predict the variation to be benign; this allele is also relatively common in the South Asian population (MAF 11%). Thus, it seems not likely to be a pathogenic variant.
ATP8B1 variants
Several variants of interest were identified in ATP8B1, encoding a phosphatidyl serine flippase. A mutation predicted to be pathogenic by SIFT and Mutation Taster, causing the protein change Asn45Thr, was seen in 3 unrelated individuals. Two further variants predicted to be pathogenic were identified in 2 additional patients, resulting in the protein changes Glu114Gln and Lys203Glu. To clarify the potential pathogenic and recurrent role (in ICP) of the Asn45Thr variant a cohort of 545 cases was screened for this change (see methods above); an additional 3 patients harbouring this variant were identified (Tables 1 and 2).
ABCC2 variants
Two significant alterations were identified in ABCC2, encoding MRP2, a transporter of conjugated bilirubin and other organic anions. A single missense substitution, predicted to result in the protein change Glu1352Ala was identified in one patient. Alamut analysis indicated that SIFT and mutationTaster both predict the change to be deleterious. A second identified DNA change, confirmed by RT-PCR dosage methodology, was a genomic duplication of 5299 base pairs, encompassing exons 24 and 25 of the gene and predicted to result in the insertion of a premature stop codon. This copy number variant has been reported once before (database reference esv3423829).
TJP2 variants
Three patients harboured TJP2 variants of potential interest. Two unrelated individuals had the same DNA mutation causing the protein change Thr62Met. This alteration is predicted to be disease causing by Mutation Taster; SIFT, however, predicts this change to be tolerated. A second missense alteration seen in one patient is predicted to cause the protein alteration Thr626Ser. This change is also assessed as tolerated by SIFT but as disease causing by Mutation Taster. 545 ICP cases (as above) were subsequently screened for the possible recurrent Thr62Met variant, however no further ICP cases carrying this change were identified.
Biochemical and clinical features of ICP cases with variants
Elevations in serum BA and alanine transaminase (ALT) activity values varied among patients and there was no particular trend for greater elevation of specific analytes in women with particular mutations in specific genes. Hyperbilirubinaemia was rare. It did, however, occur in association with ABCB4, ABCB11 or ATP8B1 variants. Six women had elevated bilirubin values (>20 µmol/L); all had severe ICP (serum BA > 40 µmol/L). The two whose bilirubin concentrations were consistent with jaundice (>35 µmol/L) harboured ABCB4 mutations. Only two women with mutations (one in ABCB4, one in ATP8B1) were known to have elevated gamma glutamyl transferase (GGT) levels. Of the 26 women with a mutation in a biliary transporter (ABCB4, ABCB11, APT8B1, ABCC2), 12 (46%) had an established family history of biliary disease (ICP, cirrhosis or gallstones).
Discussion
This study is the largest analysis to date of the role of mutations of familial cholestasis genes in ICP susceptibility. Previous studies have identified genetic contributions to the disease primarily focussing on ABCB4. Here, by using a next generation sequencing approach, a panel of genes could be analysed in parallel in a large cohort of patients.
Our analysis identified a number of mutations of ABCB4, encoding the phosphatidyl choline floppase MDR3. ABCB4 has been analysed in a number of ICP cohorts and mutations in this gene represent the largest overall genetic contribution to ICP susceptibility known to date15. Several groups have established functional assays for this protein that can incorporate mutant constructs43,44,45,46. Such assays help to define the impact of a given variant on protein function; bioinformatics predictors of clinical importance of variants like those used in this study are useful (and improving) but can never be conclusive. Functional assays are being used to classify mutations by mechanism of effect on protein function (e.g., trafficking defect resulting in mis-localisation, loss of floppase activity). This is of value in ABCB4-associated diseases; these data may predict response to therapy intended to rescue floppase function. It is noteworthy that in the ABCB4 mutant carrier group, 8/12 (67%) had a family history of biliary disease (ICP, cholelithiasis or cirrhosis) (Table 2). This is consistent with a study of parous women with LPAC and co-existing ABCB4 mutations, in which approximately 50% developed ICP when pregnant47.
A clear role is now established for genetic variation in ABCB11 contributing to the aetiology of ICP, although one seemingly less than that of ABCB4. Our study has confirmed this role; taken together with other data, it suggests that up to 5% of ICP cases harbour a heterozygous mutation of ABCB11 28,29,30. In particular, the two mutant alleles found commonly in the PFIC2/BRIC2 population (Glu297Gly and Asp482Gly) are also present in the ICP population. Functional studies of ABCB11 mutations have been performed in addition to mini-gene construct splicing analysis and immunohistochemical studies to establish genotype/phenotype correlations48,49,50; studies of this type are helpful to clarify the clinical relevance of findings of unknown significance. Two of the five women in this group had cholelithiasis (Table 2). Previous studies of ICP patients and ABCB11 mutations have not identified this association.
Analysis of ATP8B1 in ICP has been limited, with the largest study focussing on common SNPs and population risk rather than mutations [31–33]. In this study we confirmed a small potential role for ATP8B1 variants to contribute to ICP. We examined a larger ICP population for the recurrent variant (Asn45Thr) and identified three further individuals harbouring it. Taken with the other mutations identified in this gene, it is therefore possible that up to 3% of ICP patients may have a heterozygous mutation of ATP8B1. However, the Asn45Thr variant, although predicted to be deleterious, is fairly common in the normal population (global minor allele frequency 0.49%), and has been reported in a study of chronic pancreatitis51. Although this does not exclude this variant from having a mildly deleterious effect on protein function, in vitro experimental approaches are warranted to confirm if this variant contributes to disease risk.
That our cohort included two patients with potentially pathogenic variants of ABCC2, a missense mutation predicted to be pathogenic and a large in-frame duplication, is of interest. No published studies report sequencing this gene in ICP; our data suggest a small but potentially overlooked contribution to ICP by heterozygous ABCC2 mutations.
This study is the first to examine TJP2 in an ICP cohort. We have identified some evidence for involvement of this gene, with three occurrences of variants that may predispose to disease. However, as bioinformatics prediction tools did not agree on the clinical relevance of these changes, further analysis is warranted. Development of functional assays for this protein, together with further sequencing of TJP2 in larger patient cohorts, will be key to understanding the role of these variants.
A spectrum of variants have been identified in this and other ICP cohorts. Although some variants will be predicted to have only a mild impact upon disease susceptibility, either from database predictions or using in vitro assays, the cholestatic impact of gestational elevations of reproductive hormones may result in a more severe phenotype in the context of pregnancy.
Heterozygous mutations in the five genes sequenced were identified in nearly 20% of the ICP population being studied. However, the mutant-carrying groups exhibited no clear phenotypic differences (Table 2). Serum BA or ALT values did not vary by gene and raised serum GGT activity was not common in those with a mutation in ABCB4. Biomarkers that indicate which biliary transporter is mutated in a specific ICP patient thus remain to be found. That >50% of the women with identified variants had a family history of biliary disease is noteworthy; this information could be useful in a clinical setting to make decisions about mutation screening. Further studies with deeper phenotyping approaches (especially metabolic profiling/serum lipidomics and reproductive hormone metabolite analysis, based on our knowledge of disease pathophysiology) are warranted to determine if these mutation groups can be distinguished by clinical phenotype. Research into the impact of specific genotypes on drug response, risk of subsequent hepatobiliary disease, resolution of symptoms after delivery, duration of symptoms, and long term maternal and child health will be of particular value.
In this study, we used a candidate sequencing approach to identify mutations with a potentially large impact on protein function. Separate studies have also taken a population genetics approach using candidate single nucleotide polymorphisms and/or tagging SNPs in an attempt to identify common variants that contribute to overall risk31,38,52,53. Common variants that make a much smaller contribution to disease risk in ICP populations have been identified at the ABCB4 and ABCB11 loci (in particular rs2109505 (ABCB4) and rs2287622/rs7577650 (ABCB11)28,31,53). Thus, the genetic architecture of ICP is complex, with rare mutant alleles, often but not exclusively specific to each patient, present in affected women, such as reported in this study, together with common variants at the same loci that represent risk alleles as we have previously described. Although our previous study excluded a large role for common variation of ATP8B1 and ABCC2 in ICP31, studies in larger cohorts may identify variants conferring a small degree of risk (or protection), given the potential high-impact mutations of these genes identified by this study. Common variation around TJP2 causing small alterations in risk (which this study was not powered to detect) may also play a role.
We have previously studied the role of FXR variants in ICP and identified a small number of rare variants with a functional effect54. When designing this study this gene was not included in the screening panel. However, the recent identification of FXR mutations in progressive familial intrahepatic cholestasis strengthen the case for further FXR analysis in future studies of ICP55.
The catalogue of ICP-associated mutations that this analysis, and others, have established permits consideration of the possibility of precision genomic medicine. With sequencing costs falling and technology continuing to advance, to contemplate screening all of the candidate genes for ICP is now feasible, enabling genetic diagnosis that in future may allow better targeted treatment and surveillance.
Methods
Blood samples were collected in standard EDTA vacutainers and buffy coats were prepared by centrifugation using standard protocols. DNA was extracted from 200 µl of buffy coat using the Qiagen Blood mini kit (Crawley, UK). Extracted DNA was assessed for purity using an ND-1000 Nanodrop spectrophotometer (Thermofisher Scientific, Loughborough, UK) and quantified using a Qubit fluorimeter (Thermofisher).
Selected genes known or hypothesized to be involved in ICP (ABCB4, ABCB11, ATP8B1, ABCC2 and TJP2) underwent targeted next-generation sequencing. Oligonucleotides (“oligos”) to screen the entire coding region of each gene were designed using the Illumina web-based sequencing assay design tool Design Studio (http://designstudio.illumina.com/) and used in the Illumina TruSeq custom amplicon v1.5 workflow according to the manufacturer’s instructions. This workflow has three main stages: 1) hybridisation of the oligos to 50 ng/µl of genomic DNA; 2) extension and ligation of the oligos; 3) PCR amplification using two unique index primers for sample. Afterwards, sample DNA concentrations were normalised using the Illumina bead-based system and pooled in a final library. The pooled library was then sequenced using a MiSeq Reagent Kit v2, 300-cycle (2 × 150bp), on the MiSeq benchtop sequencing platform (Illumina, Cambridge, UK).
Sequencing data were analysed using a bioinformatics pipeline designed in Biomedical Genomic Workbench 2.5.1 (CLC bio, Aarhus, Denmark). Sequence reads were mapped against the human reference (hg19/GRCh37). Variants were called when they had a minimum coverage of 20× and a probability of 80% of being different from the reference, in accordance with the Bayesian model incorporated into the software. Putative variants identified were filtered according to the quality and the frequency of occurrence; all changes having an allele read frequency of less than 10% and an average base quality (Phred score) of less than 20 were removed. The variants identified were further annotated using dbSNP v139 and the 1000 Genome Project database. A deeper investigation was also performed using Alamut Visual 2.7.1 (Interactive Biosoftware, Rouen, France), in which each variant was integrated with allele frequency information derived from several single nucleotide polymorphism (SNP) databases, including dbSNP v144, the 1000 Genomes Project, the Exome Aggregation Consortium and the National Heart Lung and Blood Institute Grand Opportunity Exome Sequencing Project and with in silico missense predictions from SIFT (sorting intolerant from tolerant) and MutationTaster. Copy number variants (CNVs) were detected via in-house dosage analysis using the read-counts generated by the NGS analysis. The CNVs were confirmed by RT-PCR using Universal Probe Library (Roche).
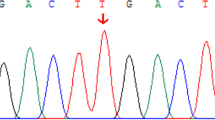
Each potential pathogenic variant was confirmed in patient samples using routine Sanger sequencing. Forward and reverse primers were manually designed for the flanking regions and purchased from Integrated DNA Technologies (sequences available on request).
Analysis of potential recurrent mutations of ATP8B1 and TJP2 were performed following primer design (“Primer picker”, LGC Genomics, Hoddesdon, UK) using a competitive allele specific PCR SNP system using fluorescence resonance energy transfer (FRET) quencher cassette oligonucleotides (KASPTM, LGC Genomics).
Data Availability
Any further information on the sequencing data described in this paper is available from the corresponding author on reasonable request.
References
Geenes, V. & Williamson, C. Intrahepatic cholestasis of pregnancy. World journal of gastroenterology 15, 2049–2066 (2009).
Fisk, N. M. & Storey, G. N. Fetal outcome in obstetric cholestasis. Br J Obstet Gynaecol 95, 1137–1143 (1988).
Williamson, C. et al. Clinical outcome in a series of cases of obstetric cholestasis identified via a patient support group. Br J Obstet Gynaecol 111, 676–681 (2004).
Walker, I. A., Nelson-Piercy, C. & Williamson, C. Role of bile acid measurement in pregnancy. Ann Clin Biochem 39, 105–113 (2002).
Glantz, A., Marschall, H. U. & Mattsson, L. A. Intrahepatic cholestasis of pregnancy: Relationships between bile acid levels and fetal complication rates. Hepatology 40, 467–474 (2004).
Geenes, V. et al. Association of severe intrahepatic cholestasis of pregnancy with adverse pregnancy outcomes: a prospective population-based case-control study. Hepatology 59, 1482–1491 (2014).
Dann, A. T. et al. Plasma lipid profiles of women with intrahepatic cholestasis of pregnancy. Obstet Gynecol 107, 106–114 (2006).
Martineau, M. G. et al. The metabolic profile of intrahepatic cholestasis of pregnancy is associated with impaired glucose tolerance, dyslipidemia, and increased fetal growth. Diabetes Care 38, 243–248 (2015).
Wikstrom Shemer, E. A. et al. Intrahepatic cholestasis of pregnancy and cancer, immune-mediated and cardiovascular diseases: A population-based cohort study. Journal of hepatology 63, 456–461 (2015).
Marschall, H. U., Wikstrom Shemer, E., Ludvigsson, J. F. & Stephansson, O. Intrahepatic cholestasis of pregnancy and associated hepatobiliary disease: a population-based cohort study. Hepatology 58, 1385–1391 (2013).
Papacleovoulou, G. et al. Maternal cholestasis during pregnancy programs metabolic disease in offspring. J Clin Invest 123, 3172–3181 (2013).
Abu-Hayyeh, S. et al. Prognostic and mechanistic potential of progesterone sulfates in intrahepatic cholestasis of pregnancy and pruritus gravidarum. Hepatology 63, 1287–98 (2015).
Song, X. et al. Transcriptional dynamics of bile salt export pump during pregnancy: mechanisms and implications in intrahepatic cholestasis of pregnancy. Hepatology 60, 1993–2007 (2014).
Abu-Hayyeh, S., Papacleovoulou, G. & Williamson, C. Nuclear receptors, bile acids and cholesterol homeostasis series - bile acids and pregnancy. Mol Cell Endocrinol 368, 120–128 (2013).
Dixon, P. H. & Williamson, C. The pathophysiology of intrahepatic cholestasis of pregnancy. Clin Res Hepatol Gastroenterol 40, 141–153 (2016).
Reyes, H., Ribalta, J. & Gonzalez-Ceron, M. Idiopathic cholestasis of pregnancy in a large kindred. Gut 17, 709–713 (1976).
Holzbach, R. T., Sivak, D. A. & Braun, W. E. Familial recurrent intrahepatic cholestasis of pregnancy: a genetic study providing evidence for transmission of a sex-limited, dominant trait. Gastroenterology 85, 175–179 (1983).
Palmer, D. G. & Eads, J. Intrahepatic cholestasis of pregnancy: a critical review. J Perinat Neonatal Nurs 14, 39–51 (2000).
Reyes, H. et al. Prevalence of intrahepatic cholestasis of pregnancy in Chile. Ann Intern Med 88, 487–493 (1978).
Eloranta, M. L., Heinonen, S., Mononen, T. & Saarikoski, S. Risk of obstetric cholestasis in sisters of index patients. Clin Genet 60, 42–45 (2001).
Dixon, P. H. & Williamson, C. The molecular genetics of intrahepatic cholestasis of pregnancy. Obstetric Medicine 1, 65–71 (2008).
van der Woerd, W. L. et al. Familial cholestasis: progressive familial intrahepatic cholestasis, benign recurrent intrahepatic cholestasis and intrahepatic cholestasis of pregnancy. Best Pract Res Clin Gastroenterol 24, 541–553 (2010).
Jacquemin, E., Cresteil, D., Manouvrier, S., Boute, O. & Hadchouel, M. Heterozygous non-sense mutation of the MDR3 gene in familial intrahepatic cholestasis of pregnancy. Lancet 353, 210–211 (1999).
Dixon, P. H. et al. Heterozygous MDR3 missense mutation associated with intrahepatic cholestasis of pregnancy: evidence for a defect in protein trafficking. Hum Mol Genet 9, 1209–1217 (2000).
Jirsa, M. et al. ABCB4 mutations underlie hormonal cholestasis but not pediatric idiopathic gallstones. World journal of gastroenterology 20, 5867–5874 (2014).
Rosmorduc, O. & Poupon, R. Low phospholipid associated cholelithiasis: association with mutation in the MDR3/ABCB4 gene. Orphanet J Rare Dis 2, 29 (2007).
Strautnieks, S. S. et al. A gene encoding a liver-specific ABC transporter is mutated in progressive familial intrahepatic cholestasis. Nat Genet 20, 233–238 (1998).
Pauli-Magnus, C. et al. Sequence analysis of bile salt export pump (ABCB11) and multidrug resistance p-glycoprotein 3 (ABCB4, MDR3) in patients with intrahepatic cholestasis of pregnancy. Pharmacogenetics 14, 91–102 (2004).
Dixon, P. H. et al. Contribution of variant alleles of ABCB11 to susceptibility to intrahepatic cholestasis of pregnancy. Gut 58, 537–544 (2008).
Anzivino, C. et al. ABCB4 and ABCB11 mutations in intrahepatic cholestasis of pregnancy in an Italian population. Dig Liver Dis 45, 226–232 (2013).
Dixon, P. H. et al. A comprehensive analysis of common genetic variation around six candidate loci for intrahepatic cholestasis of pregnancy. Am J Gastroenterol 109, 76–84 (2014).
Painter, J. N. et al. Sequence variation in the ATP8B1 gene and intrahepatic cholestasis of pregnancy. Eur J Hum Genet 13, 435–439 (2005).
Mullenbach, R. et al. ATP8B1 mutations in British cases with intrahepatic cholestasis of pregnancy. Gut 54, 829–834 (2005).
Groen, A. et al. Complementary functions of the flippase ATP8B1 and the floppase ABCB4 in maintaining canalicular membrane integrity. Gastroenterology 141, 1927–1937 (2011).
Chen, F., Ghosh, A. & Shneider, B. L. Phospholipase D2 mediates signaling by ATPase class I type 8B membrane 1. Journal of lipid research 54, 379–385 (2013).
Jemnitz, K. et al. ABCC2/Abcc2: a multispecific transporter with dominant excretory functions. Drug metabolism reviews 42, 402–436 (2010).
Sookoian, S., Castano, G., Burgueno, A., Gianotti, T. F. & Pirola, C. J. Association of the multidrug-resistance-associated protein gene (ABCC2) variants with intrahepatic cholestasis of pregnancy. J Hepatol 48, 125–132 (2008).
Meier, Y. et al. Increased susceptibility for intrahepatic cholestasis of pregnancy and contraceptive-induced cholestasis in carriers of the 1331T > C polymorphism in the bile salt export pump. World J Gastroenterol 14, 38–45 (2008).
Davit-Spraul, A. et al. ATP8B1 and ABCB11 analysis in 62 children with normal gamma-glutamyl transferase progressive familial intrahepatic cholestasis (PFIC): phenotypic differences between PFIC1 and PFIC2 and natural history. Hepatology 51, 1645–1655 (2010).
Sambrotta, M. et al. Mutations in TJP2 cause progressive cholestatic liver disease. Nat Genet 46, 326–328 (2014).
Rosmorduc, O., Hermelin, B. & Poupon, R. MDR3 gene defect in adults with symptomatic intrahepatic and gallbladder cholesterol cholelithiasis. Gastroenterology 120, 1459–1467 (2001).
Bacq, Y. et al. ABCB4 gene mutations and single-nucleotide polymorphisms in women with intrahepatic cholestasis of pregnancy. Journal of medical genetics 46, 711–715 (2009).
Andress, E. J. et al. Molecular mechanistic explanation for the spectrum of cholestatic disease caused by the S320F variant of ABCB4. Hepatology 59, 1921–1931 (2014).
Gautherot, J. et al. Phosphorylation of ABCB4 impacts its function: insights from disease-causing mutations. Hepatology 60, 610–621 (2014).
Gordo-Gilart, R. et al. Functional analysis of ABCB4 mutations relates clinical outcomes of progressive familial intrahepatic cholestasis type 3 to the degree of MDR3 floppase activity. Gut 64, 147–155 (2015).
Delaunay, J. L. et al. A functional classification of ABCB4 variations causing progressive familial intrahepatic cholestasis type 3. Hepatology 63, 1620–31 (2016).
Poupon, R. et al. Genotype-phenotype relationships in the low-phospholipid-associated cholelithiasis syndrome: a study of 156 consecutive patients. Hepatology 58, 1105–1110 (2013).
Strautnieks, S. S. et al. Severe bile salt export pump deficiency: 82 different ABCB11 mutations in 109 families. Gastroenterology 134, 1203–1214 (2008).
Byrne, J. A. et al. Missense mutations and single nucleotide polymorphisms in ABCB11 impair bile salt export pump processing and function or disrupt pre-messenger RNA splicing. Hepatology 49, 553–567 (2009).
Noe, J., Stieger, B. & Meier, P. J. Functional expression of the canalicular bile salt export pump of human liver. Gastroenterology 123, 1659–1666 (2002).
van der Woerd, W. L. et al. Mutational analysis of ATP8B1 in patients with chronic pancreatitis. PLoS One 8, e80553 (2013).
Eloranta, M. L. et al. Association of single nucleotide polymorphisms of the bile salt export pump gene with intrahepatic cholestasis of pregnancy. Scand J Gastroenterol 38, 648–652 (2003).
Wasmuth, H. E. et al. Intrahepatic cholestasis of pregnancy: the severe form is associated with common variants of the hepatobiliary phospholipid transporter ABCB4 gene. Gut 56, 265–270 (2007).
Van Mil, S. W. et al. Functional variants of the central bile acid sensor FXR identified in intrahepatic cholestasis of pregnancy. Gastroenterology 133, 507–516 (2007).
Gomez-Ospina, N. et al. Mutations in the nuclear bile acid receptor FXR cause progressive familial intrahepatic cholestasis. Nat Commun 7, 10713 (2016).
Acknowledgements
The authors wish to acknowledge the patients who participated in this study, the doctors and midwives for their help with recruitment and sample collection, and the assistance of the Institute for Liver Studies, the National Institute of Health Research Biomedical Research Centres at Imperial College London and at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. The views expressed herein are those of the authors and not necessarily those of the NHS, NIHR or the Department of Health. The authors are grateful for helpful discussions with Kenneth Linton and Pierre Foskett. Financial support: The Lauren Page Trust, ICP support, Institute of Liver Studies, Wellcome Trust (P30874), National Institute of Health Research Biomedical Research Centres at the Guy’s and St Thomas’ NHS foundation Trust and the Imperial College Healthcare NHS Trust.
Author information
Authors and Affiliations
Contributions
Study conception A.K., P.H.D., C.W., R.J.T. Study design P.H.D., M.S., R.J.T., C.W. Laboratory work and analysis P.H.D., M.S., P.T-H. Patient recruitment J.C. Manuscript preparation P.H.D. All authors critically reviewed the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dixon, P.H., Sambrotta, M., Chambers, J. et al. An expanded role for heterozygous mutations of ABCB4, ABCB11, ATP8B1, ABCC2 and TJP2 in intrahepatic cholestasis of pregnancy. Sci Rep 7, 11823 (2017). https://doi.org/10.1038/s41598-017-11626-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-11626-x
This article is cited by
-
Miscarriage risk assessment: a bioinformatic approach to identifying candidate lethal genes and variants
Human Genetics (2024)
-
Rare variant contribution to cholestatic liver disease in a South Asian population in the United Kingdom
Scientific Reports (2023)
-
ABCB4 Mutations in Adults Cause a Spectrum Cholestatic Disorder Histologically Distinct from Other Biliary Disease
Digestive Diseases and Sciences (2022)
-
GWAS meta-analysis of intrahepatic cholestasis of pregnancy implicates multiple hepatic genes and regulatory elements
Nature Communications (2022)
-
Whole-exome sequencing identifies novel mutations in ABC transporter genes associated with intrahepatic cholestasis of pregnancy disease: a case-control study
BMC Pregnancy and Childbirth (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.


