Abstract
Background
There are insufficient data to make firm dietary recommendations for patients with inflammatory bowel disease (IBD). Yet patients frequently report that specific food items influence their symptoms. In this study, we describe patients’ perceptions about the benefits and harms of selected foods and patients’ dietary patterns.
Methods
CCFA Partners is an ongoing internet-based cohort study of patients with IBD. We used a semi-quantitative food frequency questionnaire to measure dietary consumption patterns and open-ended questions to elicit responses from patients about food items they believe ameliorate or exacerbate IBD. We categorized patients into four mutually exclusive disease categories: CD without an ostomy or pouch (CD), UC without an ostomy or pouch (UC), CD with an ostomy (CD-ostomy), and UC with a pouch (UC-pouch).
Results
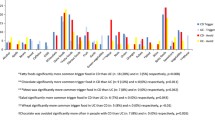
Yogurt, rice, and bananas were more frequently reported to improve symptoms whereas non-leafy vegetables, spicy foods, fruit, nuts, leafy vegetables, fried foods, milk, red meat, soda, popcorn, dairy, alcohol, high-fiber foods, corn, fatty foods, seeds, coffee, and beans were more frequently reported to worsen symptoms. Compared to CD patients, CD-ostomy patients reported significantly greater consumption of cheese (odds ratio [OR] 1.56, 95 % CI 1.03–2.36), sweetened beverages (OR 2.14, 95 % CI 1.02–1.03), milk (OR 1.84, 95 % CI 1.35–2.52), pizza (OR 1.57, 95 % CI 1.12–2.20), and processed meats (OR 1.40; 95 % CI 1.04–1.89).
Conclusions
Patients identified foods that they believe worsen symptoms and restricted their diet. Patients with ostomies ate a more liberal diet. Prospective studies are needed to determine whether diet influences disease course.
Similar content being viewed by others
References
Hwang C, Ross V, Mahadevan U. Micronutrient deficiencies in inflammatory bowel disease: from A to zinc. Inflamm Bowel Dis. 2012. doi: 10.1002/ibd.22906. [Epub ahead of print]
Harries AD, Heatley RV. Nutritional disturbances in Crohn’s disease. Postgrad Med J. 1983;59:690–697.
Saibeni S, Cortinovis I, Beretta L, et al. Gender and disease activity influence health-related quality of life in inflammatory bowel diseases. Hepatogastroenterology. 2005;52:509–515.
Casellas F, Lopez-Vivancos J, Badia X, Vilaseca J, Malagelada JR. Influence of inflammatory bowel disease on different dimensions of quality of life. Eur J Gastroenterol Hepatol. 2001;13:567–572.
Lewis JD, Fisher RL. Nutrition support in inflammatory bowel disease. Med Clin North Am. 1994;78:1443–1456.
Hou JK, Abraham B, El-Serag H. Dietary intake and risk of developing inflammatory bowel disease: a systematic review of the literature. Am J Gastroenterol. 2011;106:563–573.
Gentschew L, Ferguson LR. Role of nutrition and microbiota in susceptibility to inflammatory bowel diseases. Mol Nutr Food Res. 2012;56:524–535.
Cottone M, Orlando A, Modesto I. Postoperative maintenance therapy for inflammatory bowel disease. Curr Opin Gastroenterol. 2006;22:377–381.
Teahon K, Smethurst P, Pearson M, Levi AJ, Bjarnason I. The effect of elemental diet on intestinal permeability and inflammation in Crohn’s disease. Gastroenterology. 1991;101:84–89.
Dignass A, Van Assche G, Lindsay JO, et al. The second European evidence-based consensus on the diagnosis and management of Crohn’s disease: current management. J Crohns Colitis. 2010;4:28–62.
Rajendran N, Kumar D. Food-specific IgG4-guided exclusion diets improve symptoms in Crohn’s disease: a pilot study. Colorectal Dis. 2011;13:1009–1013.
Brown AC, Rampertab SD, Mullin GE. Existing dietary guidelines for Crohn’s disease and ulcerative colitis. Expert Rev Gastroenterol Hepatol. 2011;5:411–425.
Bando M, Hiroshima Y, Kataoka M, et al. Modulation of calprotectin in human keratinocytes by keratinocyte growth factor and interleukin-1alpha. Immunol Cell Biol. 2010;88:328–333.
Long MD, Kappelman MD, Martin CF, et al. Development of an internet-based cohort of patients with inflammatory bowel diseases (CCFA Partners): methodology and initial results. Inflamm Bowel Dis. 2012. doi: 10.1002/ibd.22895.
Jowett SL, Seal CJ, Pearce MS, et al. Influence of dietary factors on the clinical course of ulcerative colitis: a prospective cohort study. Gut. 2004;53:1479–1484.
Ballegaard M, Bjergstrom A, Brondum S, Hylander E, Jensen L, Ladefoged K. Self-reported food intolerance in chronic inflammatory bowel disease. Scand J Gastroenterol. 1997;32:569–571.
Riordan AM, Hunter JO, Cowan RE, et al. Treatment of active Crohn’s disease by exclusion diet: East Anglian multicentre controlled trial. Lancet. 1993;342:1131–1134.
Eadala P, Matthews SB, Waud JP, Green JT, Campbell AK. Association of lactose sensitivity with inflammatory bowel disease—demonstrated by analysis of genetic polymorphism, breath gases and symptoms. Aliment Pharmacol Ther. 2011;34:735–746.
Galvez J, Rodriguez-Cabezas ME, Zarzuelo A. Effects of dietary fiber on inflammatory bowel disease. Mol Nutr Food Res. 2005;49:601–608.
MacDermott RP. Treatment of irritable bowel syndrome in outpatients with inflammatory bowel disease using a food and beverage intolerance, food and beverage avoidance diet. Inflamm Bowel Dis. 2007;13:91–96.
Zallot C, Quilliot D, Chevaux JB, et al. Dietary beliefs and behavior among inflammatory bowel disease patients. Inflamm Bowel Dis. 2012. doi: 10.1002/ibd.22965. [Epub ahead of print]
Filippi J, Al-Jaouni R, Wiroth JB, Hebuterne X, Schneider SM. Nutritional deficiencies in patients with Crohn’s disease in remission. Inflamm Bowel Dis. 2006;12:185–191.
Vagianos K, Bector S, McConnell J, Bernstein CN. Nutrition assessment of patients with inflammatory bowel disease. JPEN J Parenter Enteral Nutr. 2007;31:311–319.
Willett W. Issues in analysis and presentation of dietary data. In: Willett W, ed. Nutritional epidemiology. New York: Oxford University Press; 1998:321–345.
Acknowledgments
This work was supported by a grant from the Crohn’s and Colitis Foundation of America for development of the CCFA Partners cohort (RSS) and in part by a Career Development Award from the Crohn’s and Colitis Foundation of America (MDL) and grants from the National Institutes of Health: K08 DK088957 (MDK), K24 DK DK078228 (JDL), and T32-DK007740 (DL).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cohen, A.B., Lee, D., Long, M.D. et al. Dietary Patterns and Self-Reported Associations of Diet with Symptoms of Inflammatory Bowel Disease. Dig Dis Sci 58, 1322–1328 (2013). https://doi.org/10.1007/s10620-012-2373-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2373-3